Publicly Funded Paxlovid
This topic is intended for Independent pharmacies only and is not applicable to Rexall pharmacies.
Select the appropriate tab to learn about publicly funded Paxlovid in your province.
British Columbia pharmacies are eligible to provide Paxlovid for eligible patients at no cost.
-
Patient eligibility is outlined on the Government of British Columbia website.
Paxlovid DINs and PINs
Table 1. Paxlovid DINs and PINs.
| DIN/PIN | Drug Name | Fee |
|---|---|---|
| 2524031 | PAXLOVID 300&100mg | $10 |
| 2527804 | PAXLOVID 150&100mg | $10 |
Submitting a Paxlovid Claim
Use the dropdowns below to learn more about submitting claims for each type of service.
-
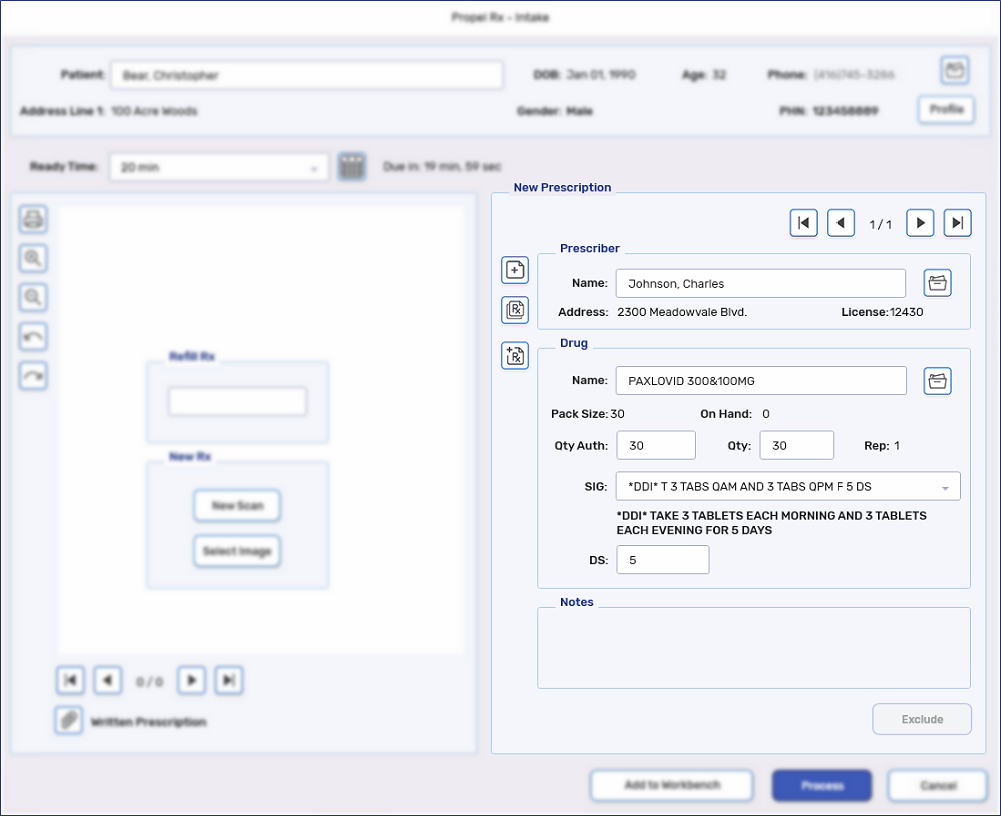
From the Workbench or patient's Profile, select Intake.
-
Enter the following information:
-
Drug = applicable DIN from Table 1
DIN 2527804 is used for patients with moderate renal impairment.
-
Qty Auth = 30 for DIN 2524031, 20 for DIN 2527804
-
Qty = 30 for DIN 2524031, 20 for DIN 2527804
-
SIG
-
DS = 5
-
-
Select Process. The prescription opens in Rx Detail.
-
Confirm the dispensing fee is not more than $10.
-
Select the Third Party tab. Confirm the TP Qty is 1.
-
Select Fill.
If during your clinical assessment, you decide to not fill the prescription, you can submit a refusal to fill fee.
-
Fill a Paxlovid prescription.
-
Refuse the prescription.
-
Refill the prescription.
-
In the Rx Detail Third Party tab, dropdown the Special Services field and select Refuse to Fill Prescription.
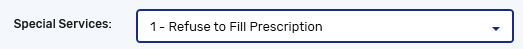
-
In the Special Service Fee field, enter up to double your pharmacy's dispensing fee.
-
Enter the appropriate intervention code. See Special Services Fees for a list of intervention codes that can be used.
-
Select Fill.
Alberta pharmacies are eligible to provide Paxlovid for eligible patients at no cost.
-
Patient eligibility is outlined on the Paxlovid Reference Guide.
-
It is not recommended for pharmacists to prescribe Paxlovid.
-
Inventory must be recorded on the Alberta Blue Cross website.
Paxlovid DIN
Table 1. Paxlovid DIN.
| DIN/PIN | Drug Name | Fee |
|---|---|---|
| 2524031 | PAXLOVID 300&100mg | Up to $22.15 |
Setting Up the Patient Folder
Claims for Paxlovid should be billed using the patient's PHN. If the patient is from out-of-province, a pseudo-PHN should be used. Select the dropdowns below for more information.
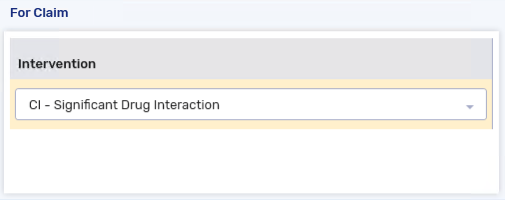
To bill a publicly funded fee for service claim for a resident of Alberta who has a valid PHN, the following Third Party information must be added to the patient’s Third Party tab:
-
Bill Code = AV (Alberta Blue Cross - Alberta Public Health Activities Program)
-
Cardholder = The first 5 characters of the patient's last name (entering the patient's complete last name is also acceptable)
-
Relationship = Card Holder
-
Carrier ID = 16
-
Group ID = 0023464000
-
Client ID = patient's PHN
To bill a publicly funded fee for service claim for a resident of Alberta without a PHN or for an out-of-province patient, the following Third Party information must be added to the patient’s Third Party tab:
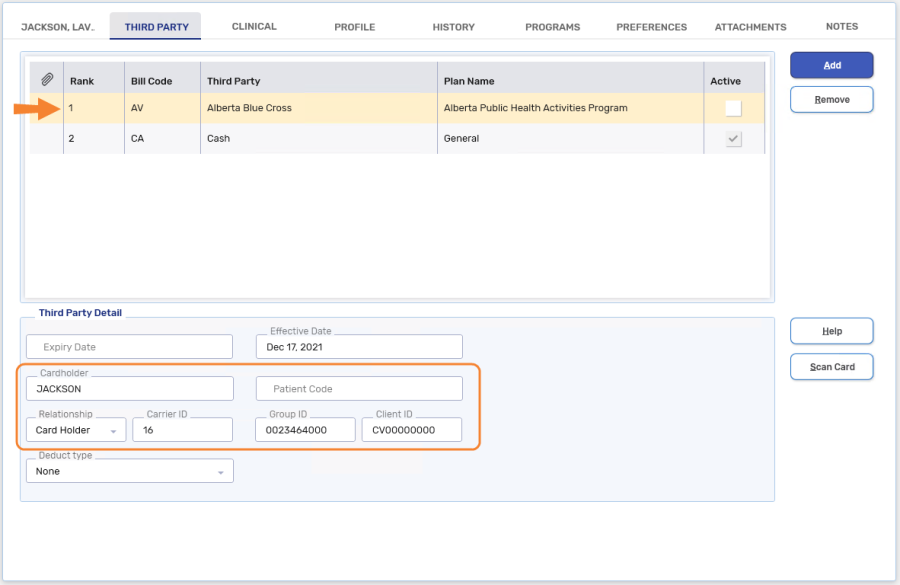
-
Bill Code = AV (Alberta Blue Cross - Alberta Public Health Activities Program)
-
Cardholder = The first 5 characters of the patient's last name (entering the patient's complete last name is also acceptable)
-
Relationship = Card Holder
-
Carrier ID = 16
-
Group ID = 0023464000
-
Client ID = CV00000000 (this is a pseudo-PHN)
When the patient is first created, enter the pseudo-PHN CV00000000 in the PHN field located in the Main tab of the Patient Folder. This will auto-populate the Client ID.
Submitting a Claim for a Paxlovid Dispense
-
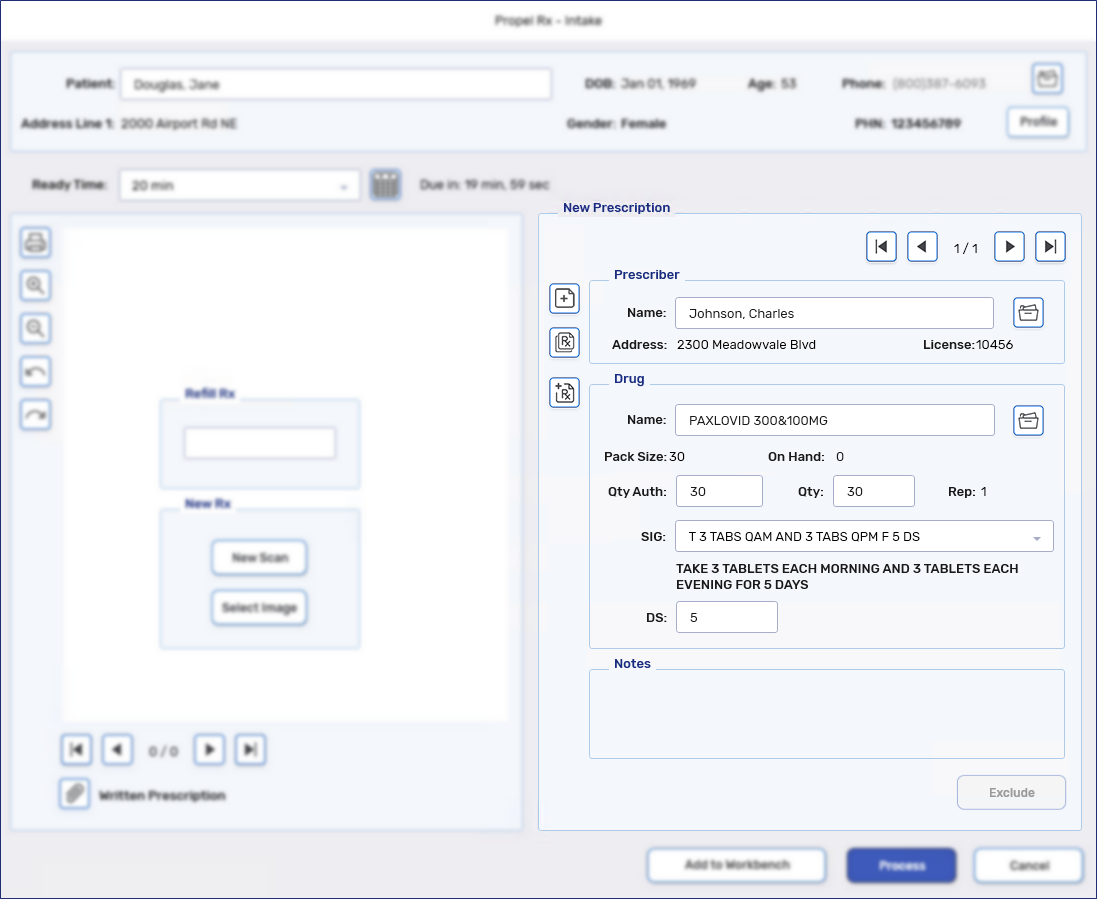
From the Workbench or patient's Profile, select Intake.
-
Enter the following information:
-
Drug = 2524031
-
Qty Auth = 30 (20 if renal impairment)
-
Qty = 30 (20 if renal impairment)
-
DS = 5
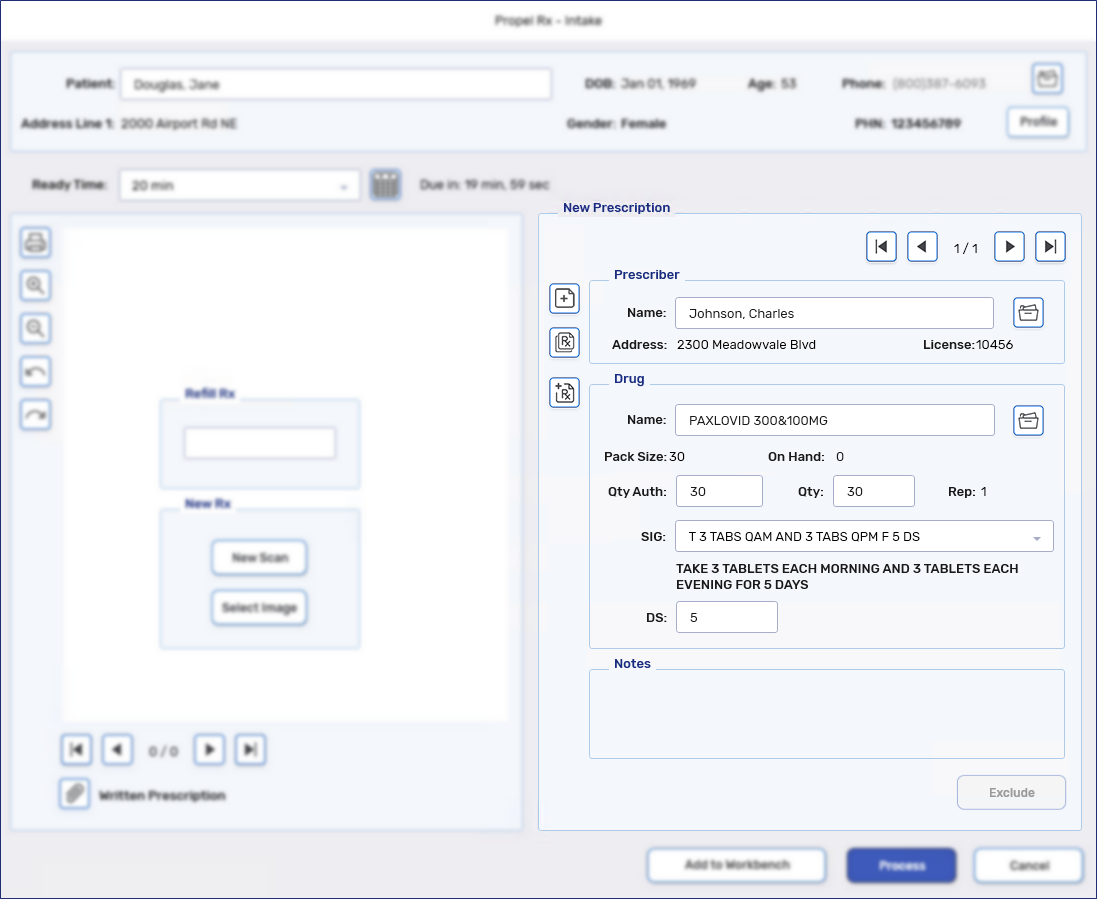
-
-
Select Process. The prescription opens in Rx Detail.
-
Enter AV/CA in the Bill field if it's not defaulted.
-
Confirm the dispensing fee is not greater than $22.15. The cost and markup should be $0.
-
Select Fill.
Last Updated: November 13, 2024
Saskatchewan pharmacies may submit the following claims related to Paxlovid therapy:
-
Assessing a patient's eligibility for Paxlovid
-
Prescribing Paxlovid under the Minor Ailment Program (patient eligibility criteria for a pharmacist issued prescription is outlined in the medSask Mild-COVID-19 Disease prescribing Guidelines)
-
Dispensing Paxlovid (refer to the DPEBB Paxlovid Distribution, Prescribing, and Assessment Program - Pharmacy Process and Billing Instructions for coverage criteria)
Paxlovid DIN and PINs
Table 1. Paxlovid DIN and PINs.
| DIN/PIN | Drug Name & Strength | Fee* |
|---|---|---|
| 2524031 | PAXLOVID 300&100mg | Acquisition cost |
| 2527804 | PAXLOVID 150&100mg | |
| 951375 | ASSESS & PRSCRBE: PAXLOVID | $25 |
| 951376 | ASSESS & PRSCRBE: PAXLOVID (REFUSAL TO FILL) PHARMACIST | |
| 951377 | ASSESS & PRSCRBE: PAXLOVID (REFUSAL TO FILL) OTHR PRSCR |
*Submitted in the Cost field of the claim.
Setting Up the Patient Folder
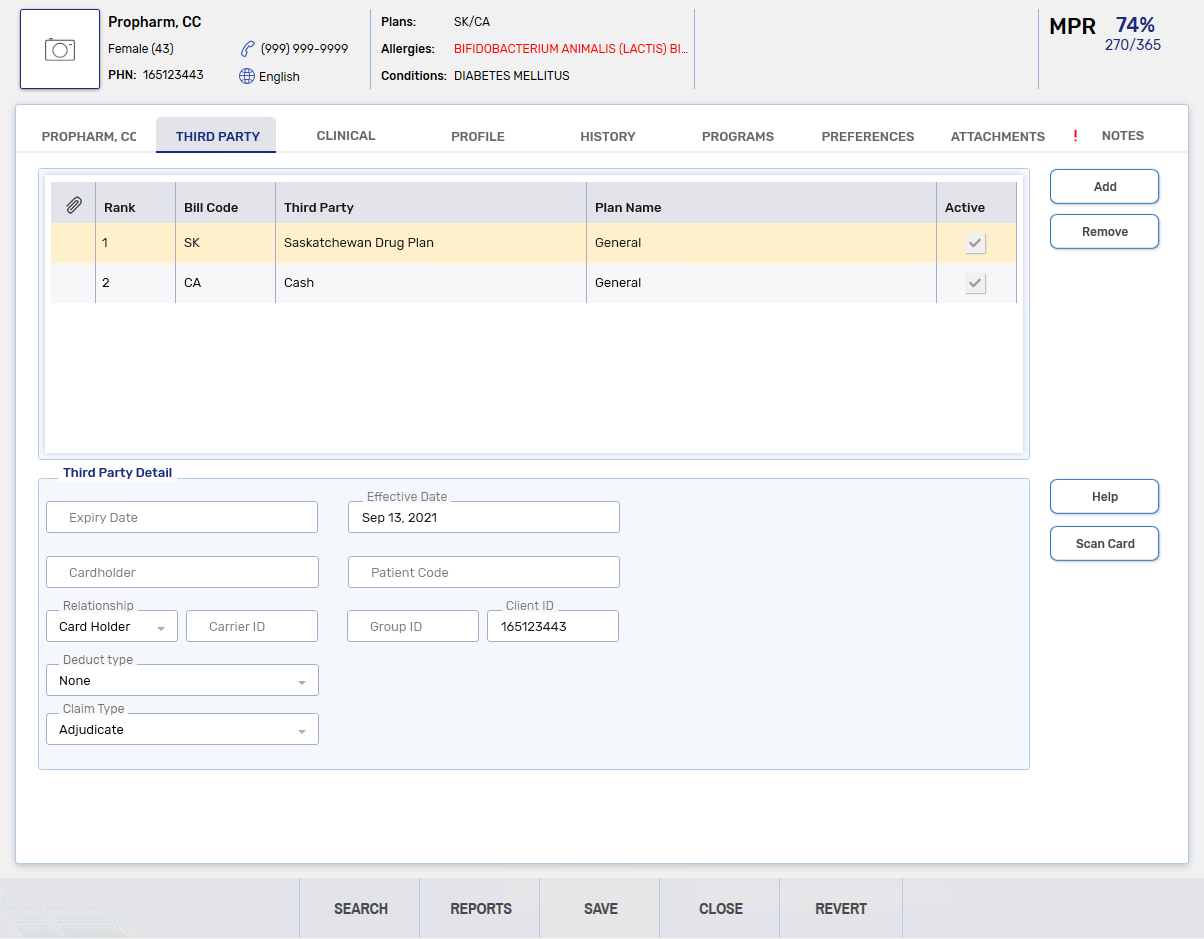
Claims must be submitted using the patient's HSN. If the patient is not a resident of Saskatchewan or has no HSN, you must contact the Drug Plan and Extended Benefits Branch (DPEBB) for further instruction.
Saskatchewan Residents with a HSN
The patient's HSN should be entered in the Client ID field for the Saskatchewan Drug Plan. The Claim Type should be set to Adjudicate.
Submitting a Paxlovid Claim
There are four types of claims that can be submitted for Paxlovid. Use the dropdowns below for more information.
-
From the Workbench or patient's Profile, select Intake.
-
Enter the following information:
-
Drug = applicable DIN
-
Qty Auth = 5
-
Qty = 5
-
DS = 5
-
-
Select Process. The prescription opens in Rx Detail.
-
The Patient EHR Access Reason window opens if the patient's EHR Profile has not been viewed yet. Select a reason for accessing the patient's EHR Profile and enter any additional comments if needed. Select OK.
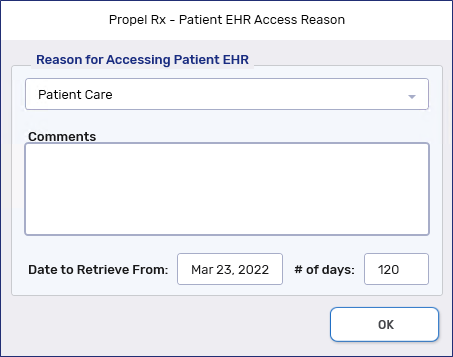
Review the patient's EHR Profile and select OK once done.
-
Select Fill.
-
If there are any Detected Issues, the Detected Issues Maintenance window opens. Review the window and add any appropriate Issue Management codes as needed.
-
Select OK.
If Paxlovid was prescribed under the Minor Ailment Program, a Minor Ailment Fee can be submitted after the Paxlovid claim has been submitted.
A maximum of 2 claims can be submitted in a 365 day period.
-
From the Workbench or patient's Profile, select Intake.
-
Enter the following information:
-
Drug = 951375
-
Qty Auth = 1
-
Qty = 1
-
DS = 1
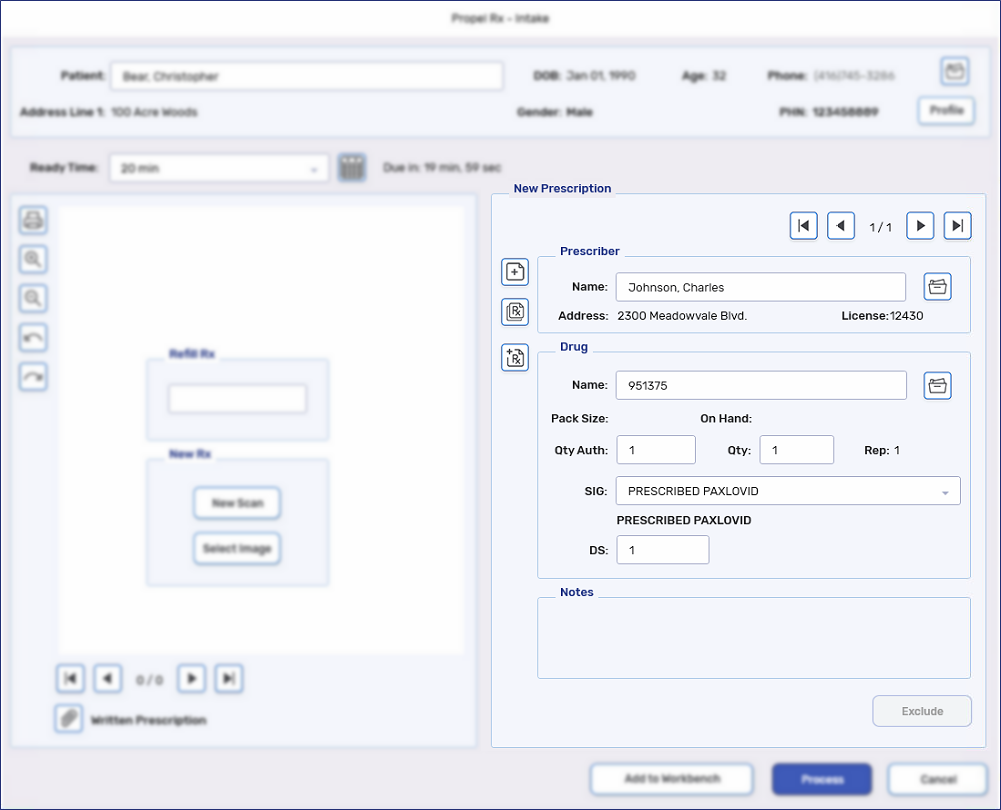
-
-
Select Process. The prescription opens in Rx Detail.
-
The Patient EHR Access Reason window opens if the patient's EHR Profile has not been viewed yet. Select a reason for accessing the patient's EHR Profile and enter any additional comments if needed. Select OK.
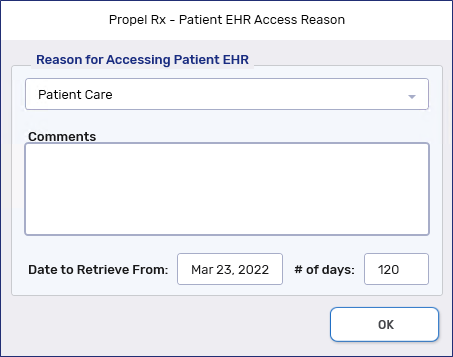
Review the patient's EHR Profile and select OK once done.
-
Confirm the cost is $25. The markup and fee should be $0.
-
Select Fill.
-
If there are any Detected Issues, the Detected Issues Maintenance window opens. Review the window and add any appropriate Issue Management codes as needed.
-
Select OK.
If the patient was deemed ineligible for Paxlovid and/or requires a referral to another health care provider, a claim can be submitted for an Ineligibility/Referral Assessment Fee.
A maximum of 2 claims can be submitted in a 365 day period.
-
From the Workbench or patient's Profile, select Intake.
-
Enter the following information:
-
Drug = 951376
-
Qty Auth = 1
-
Qty = 1
-
DS = 1
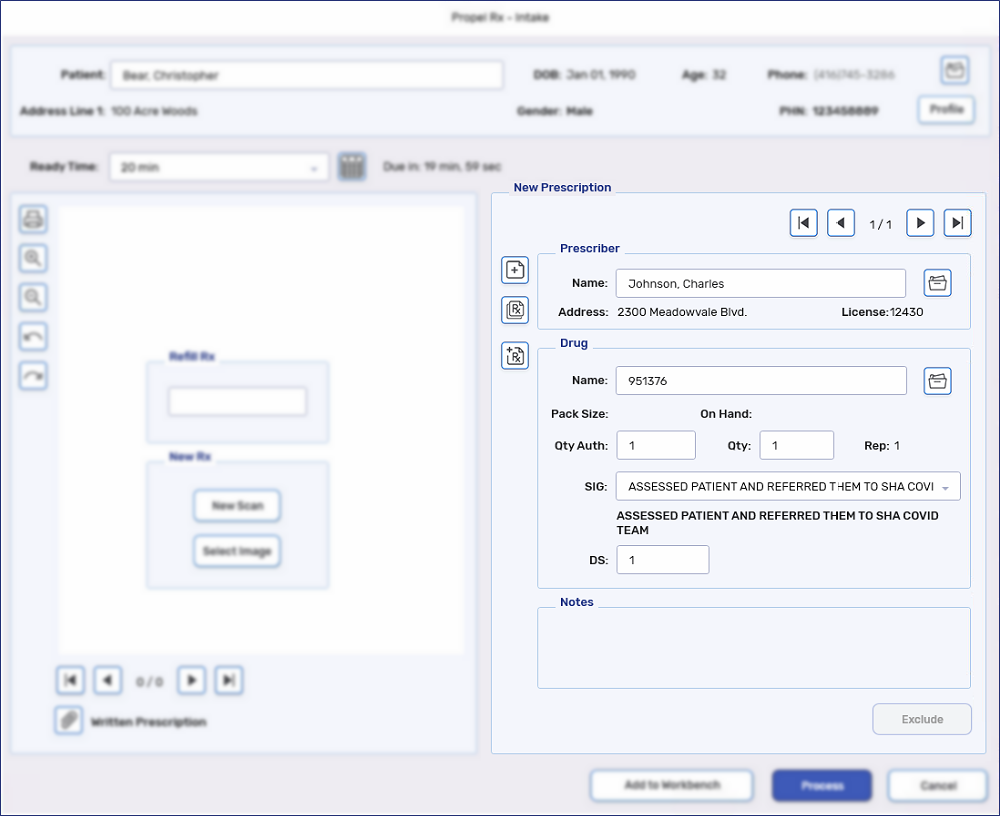
-
-
Select Process. The prescription opens in Rx Detail.
-
The Patient EHR Access Reason window opens if the patient's EHR Profile has not been viewed yet. Select a reason for accessing the patient's EHR Profile and enter any additional comments if needed. Select OK.
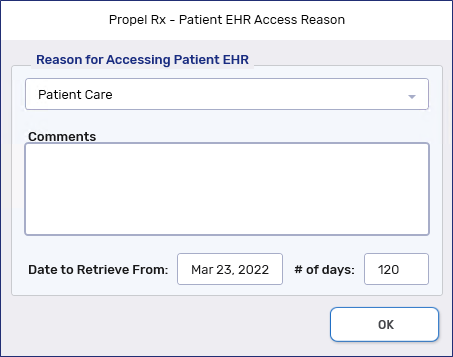
Review the patient's EHR Profile and select OK once done.
-
Confirm the cost is $25. The markup and fee should be $0.
-
Select Fill.
-
If there are any Detected Issues, the Detected Issues Maintenance window opens. Review the window and add any appropriate Issue Management codes as needed.
-
Select OK.
If a patient has a Paxlovid prescription but the patient was deemed ineligible for Paxlovid and/or requires a referral to another health care provider, a claim can be submitted for an Ineligibility/Referral Assessment Fee.
A maximum of 2 claims can be submitted in a 365 day period.
-
From the Workbench or patient's Profile, select Intake.
-
Enter the following information:
-
Drug = 951377
-
Qty Auth = 1
-
Qty = 1
-
DS = 1
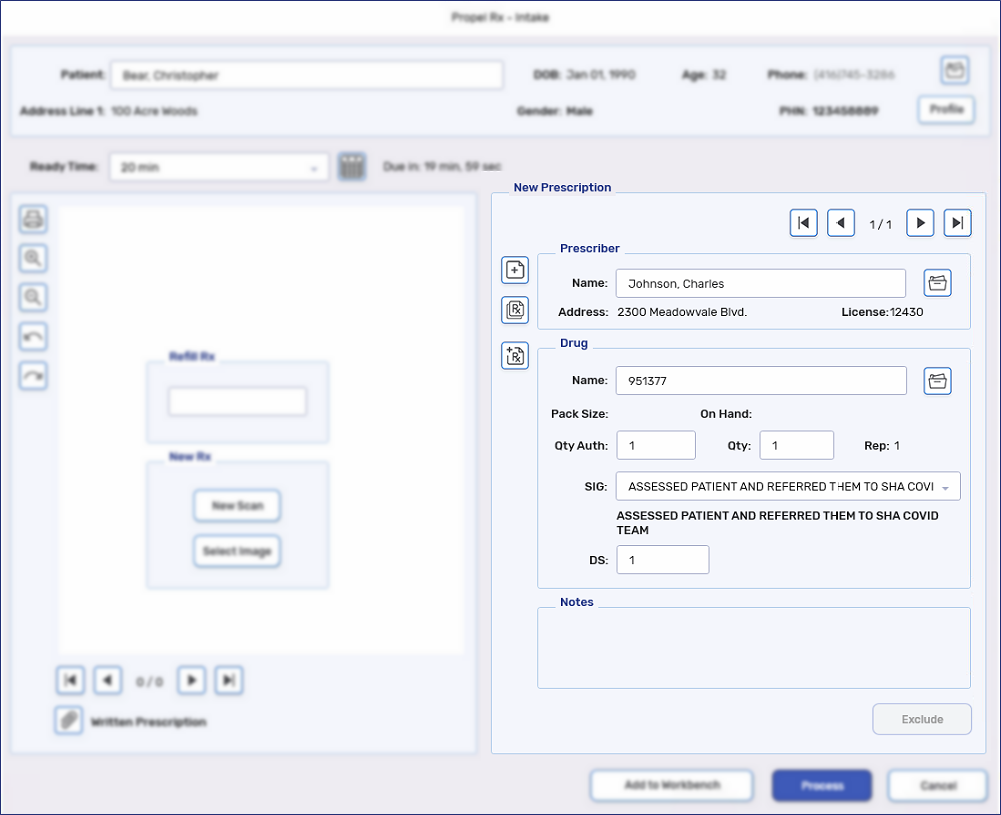
-
-
Select Process. The prescription opens in Rx Detail.
-
The Patient EHR Access Reason window opens if the patient's EHR Profile has not been viewed yet. Select a reason for accessing the patient's EHR Profile and enter any additional comments if needed. Select OK.
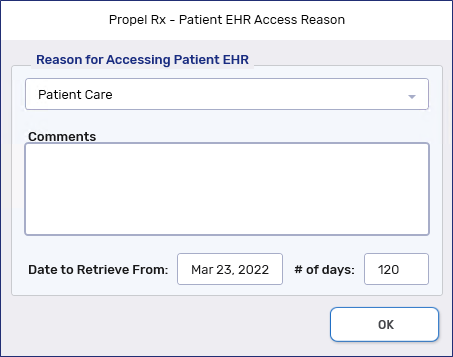
Review the patient's EHR Profile and select OK once done.
-
Confirm the cost is $25. The markup and fee should be $0.
-
Select Fill.
-
If there are any Detected Issues, the Detected Issues Maintenance window opens. Review the window and add any appropriate Issue Management codes as needed.
-
Select OK.
Last Updated: November 14, 2024
Manitoba pharmacies are eligible to provide Paxlovid at no cost to eligible patients.
-
Patient eligibility is outlined in the Claims Submission Procedure - COVID-19 Oral Antiviral Drugs (Paxlovid).
-
If a patient has coverage under a federal or provincial drug program (i.e., Personal Care Home, Employment and Income Assistance (EIA), Palliative Care), the claim should be submitted to that program instead of Public Health.
-
The patient's self-declaration of federal or provincial coverage must be documented for each dispense.
Paxlovid DIN
Table 1. Paxlovid DIN and PINs.
| DIN/PIN | Drug Name | Fee |
|---|---|---|
| 2524031 | PAXLOVID 300&100mg | Up to $14 |
| 2527804 | PAXLOVID 150&100mg |
Setting Up the Patient Folder
If a patient is eligible for Paxlovid coverage under the Manitoba Drug Benefits Formulary (MDBF), add the DM bill code to the Patient Folder Third Party tab.
-
Open the Patient Folder.
-
On the Main tab, ensure the patient’s PHIN is entered in the PHN field.
-
Select the Third Party tab.
-
Select Add.
-
Search for and select the DM bill code. The bill code details are as follows:
-
Third Party Name = Manitoba Health
-
Plan Name = Public Health
-
Carrier ID (pre-populated) = 06
-
Group ID (pre-populated) = PH
-
-
Select OK to add the plan. The Third Party Detail section should look like the image below.
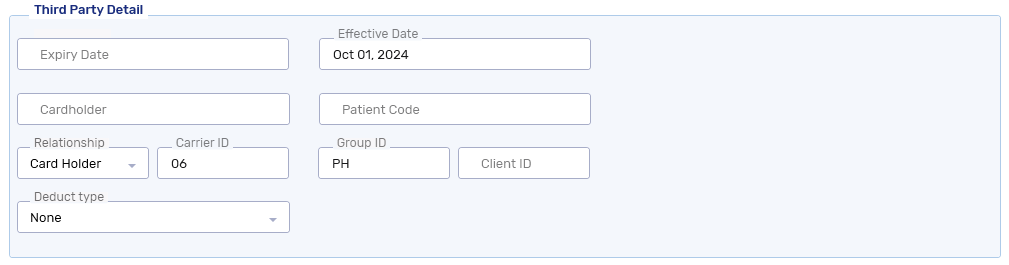
-
Select Save.
We recommend deselecting the Active checkbox for the DM bill code. By doing so, the bill code will not be added to prescriptions where it doesn’t apply.
Submitting a Paxlovid Claim
-
From the Workbench or patient's Profile, select Intake.
-
Enter the following information:
-
Drug
-
Qty Auth = 30 (20 if renal impairment)
-
Qty = 30 (20 if renal impairment)
-
DS = 5
-
-
Select Process. The prescription opens in Rx Detail.
If you set the DM bill code as Inactive in the Patient Folder, it will not auto-populate in Rx Detail; you must manually enter it in the Bill field. However, you can lock the bill code, so it carries over for future Refills.
-
Confirm the cost and markup are $0. The fee should not exceed $14.
-
Select Fill.
Ontario pharmacies may submit a claim to Ontario Drug Benefit (ODB) for the following Paxlovid related services:
-
Assessing a patient for Paxlovid therapy and issuing a prescription where appropriate.
-
Identifying a drug therapy problem related to a Paxlovid dispense and consulting with the prescriber who issued the prescription.
-
Dispensing Paxlovid pursuant to a prescription.
For more information, see the Executive Officer Notice and FAQ (dated May 17, 2024).
Paxlovid DINs and PINs
Each type of Paxlovid related service has been assigned an ODB PIN for billing purposes. Each ODB PIN has been assigned a Drug Folder in Propel Rx.
Drug Folders for Paxlovid Assessment and Prescribing
If you accessed a patient for Paxlovid therapy, submit a claim using the appropriate PIN from Table 1. The strength, or lack thereof, in the Drug Folder indicates whether the consultation was provided in-person or virtually and if it resulted in a prescription or not.
Only 1 assessment and prescribing PIN for Paxlovid and/or oseltamivir can be submitted per patient per day. If a prescription is issued, 1 claim can only be submitted for the duration of the infection(s). Check the provincial Clinical Viewers to see if a claim was already submitted for the patient.
Table 1. ODB PINs for Paxlovid assessment and prescribing services.
| PIN | Trade Name | Location? | Rx Issued? | Fee |
|---|---|---|---|---|
| 9858233 | ASSESS & PRSCRBE: PAXLOVID | In-person | Yes | $19 |
| 9858235 | ASSESS & PRSCRBE: PAXLOVID | Virtual | Yes | |
| 9858323 | ASSESS & PRSCRBE: PAXLOVID & OSELTAMIVIR | In-person | Yes | |
| 9858324 | ASSESS & PRSCRBE: PAXLOVID & OSELTAMIVIR | Virtual | Yes | |
| 9858325 | ASSESS & PRSCRBE: PAXLOVID / OSELTAMIVIR | In-person | No | |
| 9858326 | ASSESS & PRSCRBE: PAXLOVID / OSELTAMIVIR | Virtual | No |
Drug Folders for Dispensing Paxlovid
If you dispense a Paxlovid prescription, submit a claim using the appropriate DIN from Table 2.
Table 2. DINs for dispensing Paxlovid.
| Propel Rx DIN | Trade Name | Strength |
|---|---|---|
| 2524031 | PAXLOVID | 300&100MG |
| 2527804 | PAXLOVID | 150&100MG |
Drug Folders for Paxlovid Pharmaceutical Opinions
As of May 27, 2024, Paxlovid specific Pharmaceutical Opinions PINs were deactivated. The submission of Pharmaceutical Opinions for Paxlovid prescriptions will follow the same process as other drugs. For more information, see Opinions.
Setting Up the Patient Folder
Claims for Paxlovid can be submitted for three types of patients. Select the dropdowns to learn more about the billing information required for each type of patient.
To bill a publicly funded fee for service claim for an ODB-eligible patient, the following Third Party information must be added to the patient’s Third Party tab:
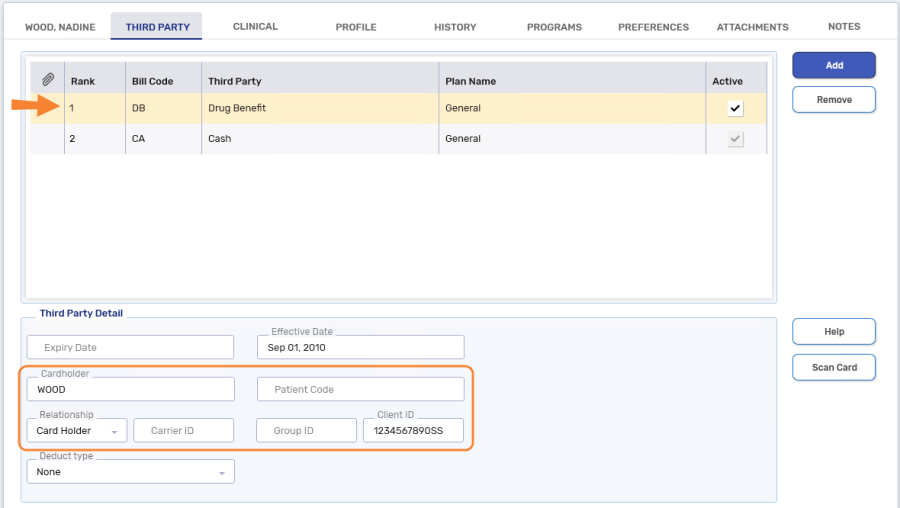
-
Bill Code = DB (Drug Benefit)
-
Cardholder = The first 5 characters of the patient's last name (entering the patient's complete last name is also acceptable)
-
Relationship = Card Holder
-
Client ID = patient's health card number
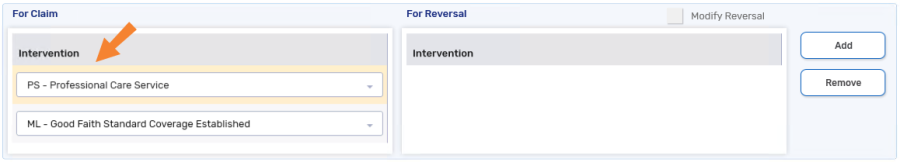
When billing the claim, the following intervention code is required in the Rx Detail > Third Party tab:
-
PS - Professional Care Service

To bill a publicly funded fee for service claim for a non-ODB recipient with a valid Ontario health card number, the following Third Party information must be added to the patient’s Third Party tab:
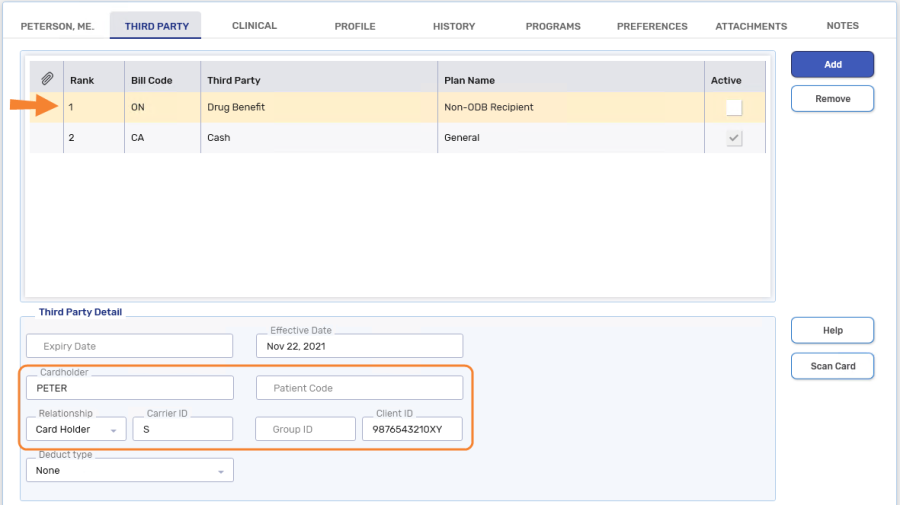
-
Bill Code = ON (Drug Benefit - Non-ODB Recipient)
- Cardholder = The first 5 characters of the patient's last name (entering the patient's complete last name is also acceptable)
-
Relationship = Card Holder
-
Carrier ID = S
-
Client ID = patient's health card number
As with all claims submitted to ODB, the patient’s gender and birth date must be recorded in the Patient Folder.
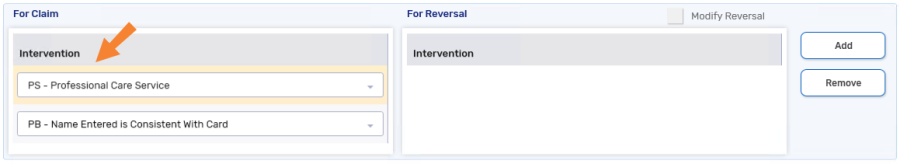
When billing the claim, the following intervention codes are required in the Rx Detail > Third Party tab:
-
PS - Professional Care Service
-
ML - Good Faith Standard Coverage
To bill a publicly funded fee for service claim for a patient without an Ontario health card number, the following Third Party information must be added to the patient’s Third Party tab:
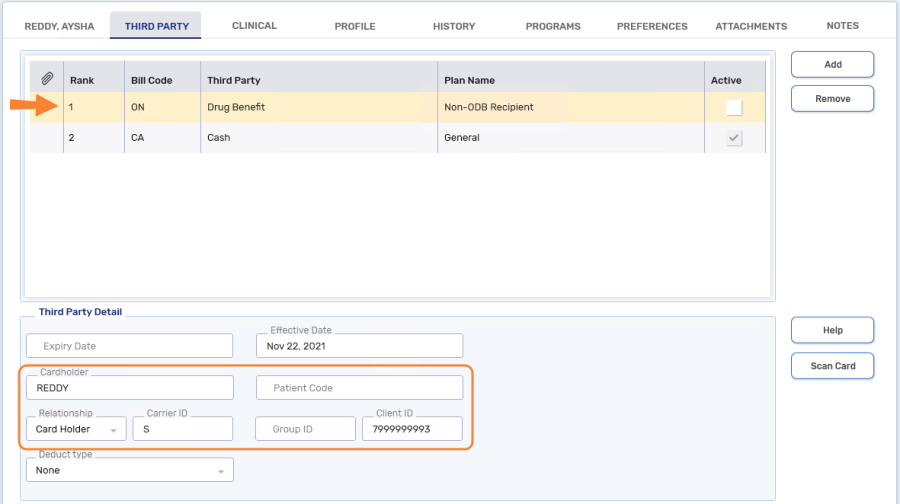
-
Bill Code = ON (Drug Benefit - Non-ODB Recipient)
- Cardholder = The first 5 characters of the patient's last name (entering the patient's complete last name is also acceptable)
Relationship = Card Holder
-
Carrier ID = S
-
Client ID = 7999999993 (this is a proxy patient ID)
As with all claims submitted to ODB, the patient’s gender and birth date must be recorded in the Patient Folder.
When billing the claim, the following intervention codes are required in the Rx Detail > Third Party tab:
-
PS - Professional Care Service
-
PB - Name Entered is Consistent With Card
Submitting a Paxlovid Claim
Use the dropdowns below for more information on how to submit the different types of Paxlovid related claims.
-
From the Workbench or patient's Profile, select Intake.
-
Enter the following information:
-
Prescriber
-
Drug = applicable DIN from Table 1
-
Qty Auth = 1
-
Qty = 1
-
SIG
-
DS
-
-
Select Process. The prescription opens in Rx Detail.
-
Confirm the cost and markup are $0. The fee should be $19.
-
Select the Third Party tab.
-
Ensure the following intervention codes are entered:
-
ODB program recipient: PS
-
Non-ODB program recipient: PS and ML
-
No Ontario Health number: PS and PB
-
-
Select Fill.
-
From the Workbench or patient's Profile, select Intake.
-
Enter the following information:
-
Drug = applicable DIN from Table 2
-
Qty Auth = 30 (20 if DIN 2527804)
-
Qty = 30 (20 if DIN 2527804)
-
DS = 5
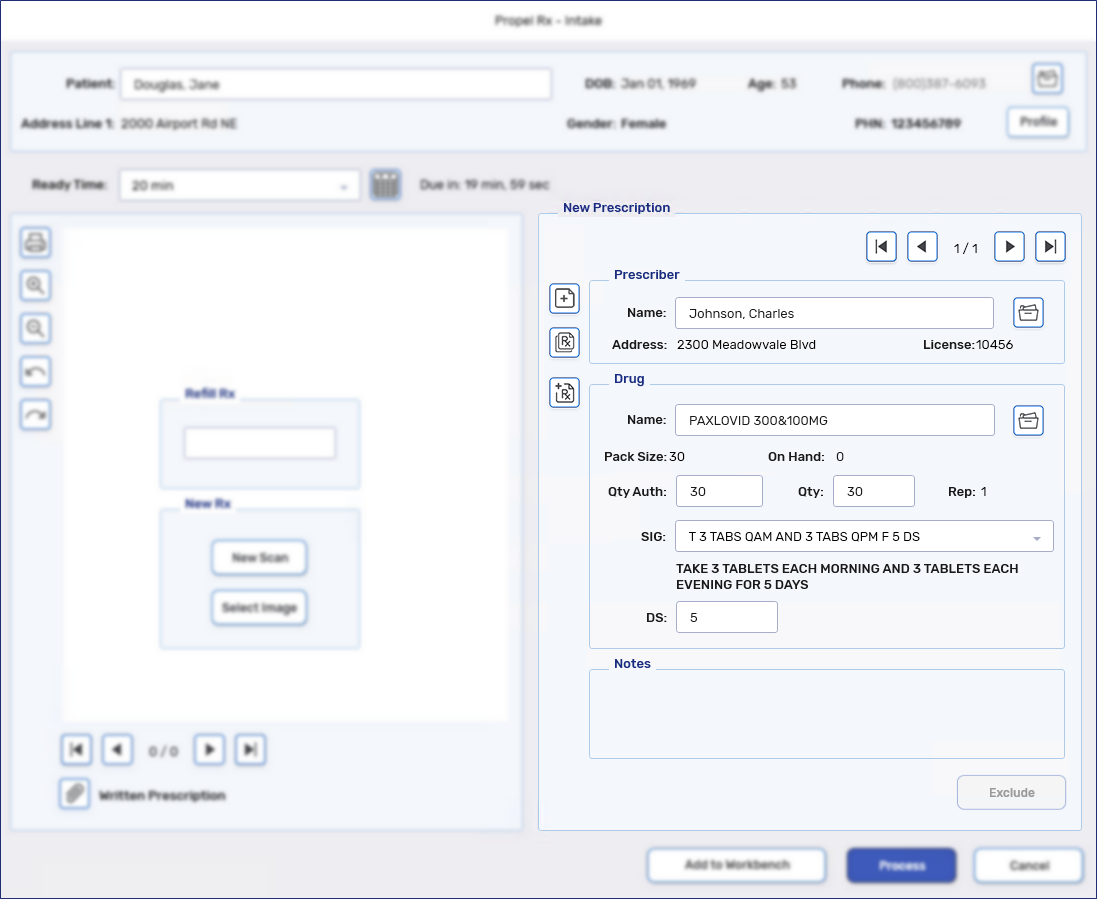
-
-
Select Process. The prescription opens in Rx Detail.
-
Select the Extended tab. Enter the applicable LU code in the MR Code field (673, 674, or 675).
-
Select the Third Party tab. Confirm the TP Qty is 1 for Ontario Drug Benefit.
-
Select Fill.